Identify and Treat Cholangitis and Cholecystitis
Learn how to identify and treat cholangitis and cholecystitis, including symptoms, causes, and treatment options. Discover how hydration plays a crucial role in recovery.
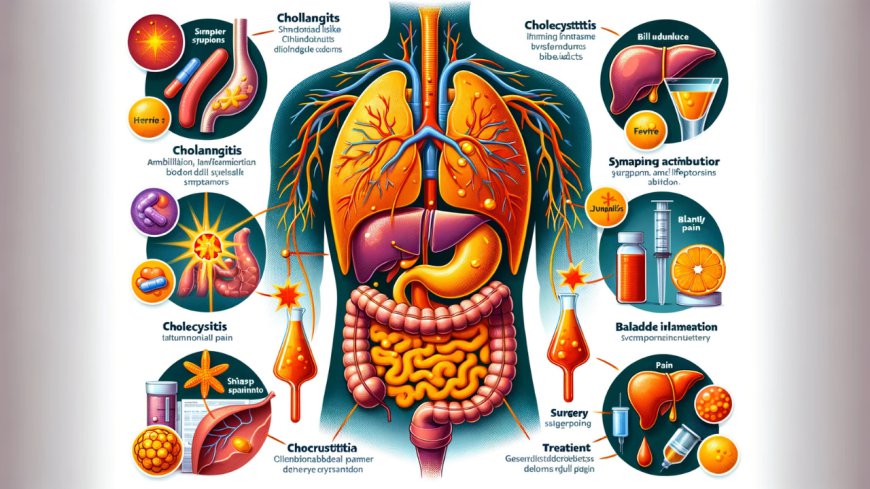
The biliary system is essential for digestion, as it transports bile from the liver and gallbladder to the small intestine. However, when this system becomes blocked or infected, it can lead to two common conditions: cholangitis and cholecystitis. These two conditions share some similarities but have key differences in their causes, symptoms, and treatment options. Knowing how to identify and treat cholangitis and cholecystitis is essential for preventing complications and promoting a quicker recovery.
In this blog, we’ll discuss how to identify cholangitis and cholecystitis, their causes, symptoms, and how to treat them effectively. We’ll also highlight the role hydration plays in managing these conditions and provide useful resources for further understanding.
What is Cholangitis?
Cholangitis is the inflammation or infection of the bile ducts. The bile ducts are tubes that carry bile from the liver and gallbladder to the small intestine, where bile helps digest fats. When the bile ducts become blocked due to gallstones, tumors, or strictures (narrowing), they can become infected, leading to cholangitis.
The most common form is acute cholangitis, also known as ascending cholangitis, which happens when bacteria travel from the intestines into the bile ducts due to an obstruction.
Symptoms of Cholangitis
Recognizing the symptoms of cholangitis early is critical for proper diagnosis and treatment. Symptoms of cholangitis may include:
- Fever with chills: A common sign of infection.
- Jaundice: Yellowing of the skin and eyes due to bile buildup.
- Right upper abdominal pain: Pain in the area around the liver, often accompanied by tenderness.
- Nausea and vomiting: These symptoms result from bile flow disruption.
- Dark urine or pale stools: Changes in urine and stool color occur due to impaired bile flow.
- Confusion or lethargy: Severe cases of cholangitis can affect mental clarity, especially in elderly patients.
These symptoms, when combined, form a classic triad known as Charcot’s triad—fever, jaundice, and right upper abdominal pain—characteristic of cholangitis.
Causes of Cholangitis
The primary cause of cholangitis is a bacterial infection. This infection usually enters the bile ducts due to:
- Gallstones: The most common cause, gallstones can block the bile ducts, allowing bacteria to enter.
- Biliary strictures: Narrowing of the bile ducts due to scar tissue or tumors.
- Tumors: Tumors may block the flow of bile, increasing the risk of infection.
- Biliary stents: Sometimes, stents placed in the bile ducts become infected.
- Pancreatic issues or surgical complications: These can lead to bile flow disruption and infection.
What is Cholecystitis?
Cholecystitis is the inflammation of the gallbladder, a small organ that stores bile. Bile is released from the gallbladder into the small intestine to help digest fats. Cholecystitis usually occurs when bile becomes trapped in the gallbladder due to a blockage, typically from gallstones. This trapped bile leads to inflammation and, in some cases, infection.
There are two main types of cholecystitis:
- Acute cholecystitis: A sudden inflammation of the gallbladder, often due to gallstones.
- Chronic cholecystitis: Long-term inflammation of the gallbladder, usually caused by repeated episodes of acute cholecystitis.
Symptoms of Cholecystitis
Symptoms of cholecystitis may overlap with those of cholangitis, but there are some key differences. Common signs of cholecystitis include:
- Severe pain in the upper right abdomen: This pain often radiates to the right shoulder or back and worsens after eating, especially after consuming fatty foods.
- Nausea and vomiting: These symptoms are common when the gallbladder is inflamed.
- Fever: This signals inflammation or infection.
- Abdominal tenderness: The area around the gallbladder may be tender, particularly after meals.
Unlike cholangitis, cholecystitis often results in more localized pain that can last several hours.
Causes of Cholecystitis
Cholecystitis occurs when bile becomes trapped in the gallbladder. The most common causes include:
- Gallstones: These block the cystic duct, causing bile to build up in the gallbladder, leading to inflammation.
- Biliary sludge: Thickened bile can block the bile ducts, leading to inflammation.
- Tumors: These can prevent bile from draining out of the gallbladder.
- Infections: Bacterial infections may also cause cholecystitis, particularly in immunocompromised individuals.
- Injury or trauma: Trauma to the gallbladder can lead to inflammation.
Identifying the Differences: Cholangitis vs Cholecystitis
Though cholangitis and cholecystitis both affect the biliary system, they differ in terms of their symptoms, causes, and areas of inflammation. Let’s examine the key differences between cholangitis vs cholecystitis:
- Location of Inflammation:
- Cholangitis: Affects the bile ducts, where bile flows from the liver to the small intestine.
- Cholecystitis: Affects the gallbladder, which stores bile before releasing it into the intestine.
- Symptoms:
- Cholangitis: Symptoms include fever, jaundice, and upper right abdominal pain (Charcot’s triad).
- Cholecystitis: Pain is the most prominent symptom, often triggered after meals and located in the upper right abdomen.
- Causes:
- Cholangitis: Caused by blockages in the bile ducts, often from gallstones or strictures, leading to infection.
- Cholecystitis: Caused primarily by gallstones blocking the cystic duct, trapping bile in the gallbladder.
For a more detailed comparison, visit cholangitis vs cholecystitis.
Treat Cholangitis and Cholecystitis: Options and Approaches
Timely treatment is crucial to prevent complications associated with cholangitis and cholecystitis. Let's explore the treatment options for each condition.
How to Treat Cholangitis
Cholangitis is a medical emergency, and treatment focuses on addressing the underlying infection and blockage. Treatment options include:
- Antibiotics: The first line of treatment involves antibiotics to combat the bacterial infection causing cholangitis.
- ERCP (Endoscopic Retrograde Cholangiopancreatography): This procedure is used to remove blockages like gallstones or tumors from the bile ducts.
- Biliary drainage: If the bile ducts are obstructed, biliary drainage may be necessary to relieve pressure and clear the infection.
- Surgery: In severe cases, surgery may be needed to remove blockages, repair the bile ducts, or treat the underlying cause.
Early intervention is crucial to prevent serious complications like liver abscesses or sepsis.
How to Treat Cholecystitis
Cholecystitis is often treated with a combination of medical management and surgery. Treatment options include:
- Antibiotics: If an infection is present, antibiotics may be prescribed to treat the inflammation.
- Cholecystectomy (Gallbladder Removal): This is the most common treatment for acute cholecystitis, especially when gallstones are involved. Cholecystectomy can be performed laparoscopically (minimally invasive) or through open surgery.
- Fasting and IV Fluids: Patients are often advised to fast to allow the gallbladder to rest, and IV fluids may be provided to prevent dehydration.
- Pain management: Pain relief medications can help alleviate the discomfort associated with gallbladder inflammation.
Cholecystectomy is a common procedure, and most people can lead healthy lives without their gallbladder.
Hydration’s Role in Recovery
Hydration is a key factor in managing both cholangitis and cholecystitis. Staying properly hydrated helps maintain healthy bile flow, preventing bile from becoming too concentrated and reducing the risk of gallstones or bile duct blockages. Dehydration can exacerbate symptoms and increase the likelihood of complications.
In addition to promoting bile flow, hydration supports liver and gallbladder function, helping the body flush out toxins and inflammation-causing agents. Drinking plenty of water is particularly important when recovering from cholangitis or cholecystitis, as it aids in healing and prevents further complications.
If you are recovering from either condition, aim to drink at least eight glasses of water daily, and avoid alcohol, which can worsen symptoms and impair recovery.
Preventing Cholangitis and Cholecystitis
While some factors like genetics and age cannot be controlled, there are steps you can take to lower your risk of cholangitis and cholecystitis. Prevention strategies include:
- Stay hydrated: Drink plenty of water to keep bile flowing smoothly and prevent the formation of gallstones.
- Eat a balanced diet: Focus on a low-fat, high-fiber diet to support gallbladder and liver health.
- Exercise regularly: Physical activity helps maintain a healthy weight and reduces the risk of gallstones.
- Avoid alcohol: Excessive alcohol consumption can damage the liver and increase the risk of infections. If you’re looking to quit alcohol, visit How To Stop Drinking Alcohol Permanently.
Conclusion
Understanding how to identify and treat cholangitis and cholecystitis is critical for preventing complications and promoting recovery. Both conditions share some similarities, but they differ in terms of symptoms, causes, and treatment options. Early diagnosis and proper treatment, combined with hydration and lifestyle adjustments, can help manage these conditions effectively.
