Transcatheter Aortic Valve Replacement: A Promising New Option for Patients With Severe Aortic Stenosis
Transcatheter aortic valve replacement (TAVR), also known as transcatheter aortic valve implantation (TAVI), is a minimally invasive procedure that repairs a diseased or damaged aortic valve without removing the old, damaged valve via open-heart surgery. TAVR offers an alternative to open-heart surgical aortic valve replacement (SAVR) for patients who are not candidates for open-heart surgery due to age, frailty, or other medical conditions.
What is Aortic Valve Stenosis?
The aortic valve controls the flow of blood from the heart to the rest of the body. Aortic stenosis occurs when the aortic valve narrows and does not open fully, obstructing blood flow from the heart into the main blood vessel (aorta). It is the most common form of valvular heart disease. Over time, the narrowed opening can prevent the heart from properly circulating blood, putting strain on the heart and reducing blood flow to the rest of the body. Left untreated, severe aortic stenosis has a poor long-term prognosis.
Who Are Candidates for TAVR?
Historically, patients with severe symptomatic aortic stenosis who were too high risk for open-heart surgery were left with limited treatment options. TAVR has emerged as a viable option for these intermediate- and high-risk patients who are not candidates for conventional surgery. Typical candidates are age 75 and older, or age 70-74 with other medical problems such as poor lung function, diabetes, or significant arthritis that adds to the risk of surgery. TAVR is not yet routinely recommended for low-risk patients who can safely undergo open-heart surgery.
How is TAVR Performed?
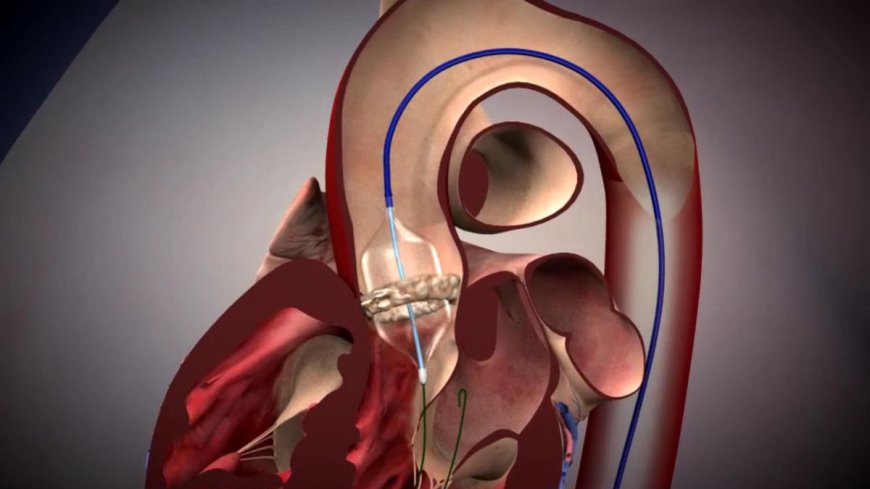
During a Transcatheter Aortic Valve Replacement [TAVR] procedure, an interventional cardiologist assesses the size and condition of the patient's heart valves via catheter-based ultrasound imaging. The cardiologist then threads a replacement valve within a compressed stent inside a catheter through an incision in the groin (femoral artery) or chest (transthoracic access) and guides it to the heart under fluoroscopic guidance. Once in place, the new valve is expanded to fix it in the proper position, pushing the old valve leaflets aside. The new valve functions immediately to restore normal blood flow. The entire procedure takes 1-2 hours to complete and does not require opening the chest or use of cardiopulmonary bypass.
Benefits of TAVR Over SAVR
The major advantages of TAVR compared to open-heart surgical aortic valve replacement include:
- Less invasive approach which avoids open-heart surgery and use of cardiopulmonary bypass. This reduces surgical risks, recovery time, pain and scarring for high-risk patients who otherwise could not tolerate open-heart surgery.
- Shorter hospital stays of only a few days versus a typical hospitalization of 1 week for SAVR. Patients can return home sooner to regain independence and mobility.
- Studies show comparable or better outcomes in mortality, stroke risk and symptom improvement at 1 year for TAVR versus SAVR in intermediate- and high-risk patients.
- TAVR offers an excellent option for valve replacement for patients with severe aortic stenosis who are considered inoperable and were previously left with few treatment options.
Types of TAVR Valves
There are currently three main transcatheter heart valves approved for use in the United States:
- Edwards Sapien valve: Made of cow tissue (bovine pericardium) mounted on a metal stent frame. Currently the market leader.
- Medtronic CoreValve: A porcine tissue (pig) valve mounted on a self-expanding nitinol stent frame.
- Boston Scientific Lotus valve: Unique design with individual petals that can reposition after placement. Made of bovine tissue mounted on a nitinol frame.
Safety and Risks of TAVR
While less invasive than open-heart surgery, TAVR is still a serious medical procedure that carries risks. Common major complications include:
- Damage to blood vessels at access site (groin or chest) requiring repair.
- Stroke from debris dislodged during the procedure, occurring in 2-4% of patients. Newer valves have led to reduced stroke rates.
- Paravalvular leak (hole in seal around new valve), requiring more procedures in 1-2% of cases.
- Pacemaker implantation occurs in 10-20% of patients due to heart block during valve placement.
- Infection of new valve requiring treatment (1-2% risk).
- Rare but serious risks of heart attack, kidney damage, or even death (2-5% 30-day mortality for high-risk patients).
Ongoing Studies and Improvements
TAVR technology is evolving rapidly. Safer transcatheter valves, novel access methods, and enhanced clinical techniques continue to emerge, driving improved outcomes. Clinical studies track long-term durability of the valves and assess the risks and benefits of TAVR in lower risk patients. As valve design and placement improve, TAVR may extend its reach to lower risk subgroups for whom SAVR would still offer strong safety today. Overall, TAVR represents an important advance in interventional cardiology that delivers life-saving valve replacement to patients previously left without good options. Continuing research aims to maximize the benefits of this promising technique.
Get More Insights - Transcatheter Aortic Valve Implantation
Discover the language that resonates with you:
· Japanese
· Korean
About Author:
Priya Pandey is a dynamic and passionate editor with over three years of expertise in content editing and proofreading. Holding a bachelor's degree in biotechnology, Priya has a knack for making the content engaging. Her diverse portfolio includes editing documents across different industries, including food and beverages, information and technology, healthcare, chemicals and materials, etc. Priya's meticulous attention to detail and commitment to excellence make her an invaluable asset in the world of content creation and refinement.

 pratikcmi
pratikcmi