Understanding Diverticulitis: A Comprehensive Guide to Managing Your Diet
Learn about diverticulitis and how to manage it through diet. Discover foods to avoid and dietary tips to alleviate symptoms and prevent flare-ups.

Understanding diverticulitis is crucial for effectively managing this common gastrointestinal condition. Diverticulitis occurs when small pouches (diverticula) in the digestive tract become inflamed or infected. While the exact cause of diverticulitis is not fully understood, diet plays a significant role in managing its symptoms and preventing flare-ups. This comprehensive guide will explain diverticulitis, its symptoms, and how to manage it through dietary changes. We will also highlight specific foods to avoid with diverticulitis and provide practical tips for maintaining a healthy diet.
Understanding Diverticulitis
Diverticulitis involves the inflammation or infection of diverticula, small pouches that can form in the walls of the colon. These pouches are common, especially in older adults, and usually don’t cause problems. However, when they become inflamed or infected, it leads to diverticulitis.
1. What Is Diverticulitis?
Diverticulitis occurs when diverticula become inflamed or infected, leading to symptoms like abdominal pain, fever, and changes in bowel habits.
- Symptoms: Common symptoms of diverticulitis include sharp abdominal pain (usually on the left side), fever, nausea, and changes in bowel habits like constipation or diarrhea. Severe cases can cause complications like abscesses, perforations, or intestinal blockages.
- Causes: The exact cause of diverticulitis is unclear, but factors like aging, low-fiber diets, and chronic constipation can contribute to the development of diverticula. When diverticula become blocked with fecal matter, bacteria can multiply, leading to inflammation or infection.
The Role of Diet in Managing Diverticulitis
Diet plays a crucial role in managing diverticulitis and preventing flare-ups. By understanding which foods to avoid and which to include, you can reduce symptoms and support overall digestive health.
1. Importance of Dietary Management
Managing diverticulitis through diet involves avoiding foods that can irritate the digestive tract and focusing on those that promote healthy digestion.
- Reducing Inflammation: Certain foods can aggravate inflammation in the colon, leading to pain and discomfort. Avoiding these foods helps reduce inflammation and prevent flare-ups.
- Promoting Healthy Digestion: A balanced diet rich in fiber supports healthy digestion and prevents constipation, reducing the risk of diverticula formation and diverticulitis.
Foods to Avoid with Diverticulitis
Understanding which foods to avoid with diverticulitis is essential for managing symptoms and preventing complications. Here are specific foods to steer clear of:
1. High-Fat Foods
High-fat foods can increase inflammation and irritate the digestive tract, leading to symptoms of diverticulitis.
- Examples: Fried foods, fatty cuts of meat, and processed snacks are high in unhealthy fats and should be avoided. These foods can slow down digestion and exacerbate symptoms.
2. Red Meat
Red meat can be difficult to digest and may contribute to inflammation in the digestive tract.
- Examples: Beef, lamb, and pork are red meats that should be limited. Instead, opt for lean proteins like chicken, turkey, or fish.
3. Dairy Products
Dairy products can cause digestive issues for some people with diverticulitis, leading to symptoms like bloating and discomfort.
- Examples: Whole milk, cream, cheese, and butter are high in fat and may irritate the digestive system. Choose low-fat or lactose-free alternatives if you tolerate them better.
4. Refined Grains
Refined grains lack fiber and can contribute to constipation, increasing the risk of diverticulitis flare-ups.
- Examples: White bread, white rice, and pastries are refined grains that should be avoided. Opt for whole grains like brown rice, whole wheat bread, and oats.
5. Certain Fruits and Vegetables
Some fruits and vegetables with seeds or skins can irritate the digestive tract and should be avoided during a diverticulitis flare-up.
- Examples: Fruits like tomatoes, strawberries, and raspberries, as well as vegetables like corn and bell peppers, can be problematic. Peel fruits and vegetables and avoid seeds when possible.
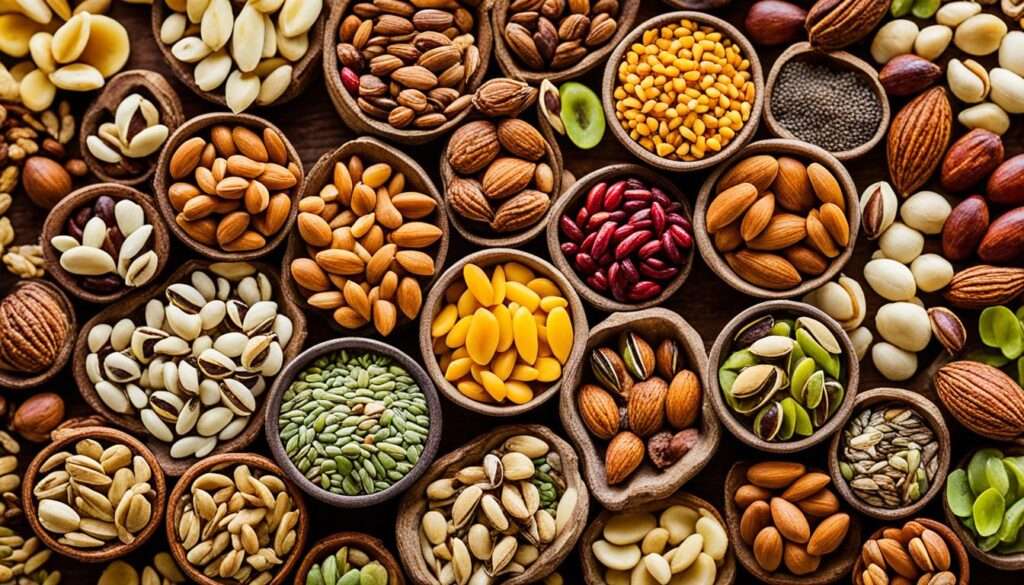
6. Nuts and Seeds
Nuts and seeds can be difficult to digest and may irritate diverticula, leading to symptoms of diverticulitis.
- Examples: Almonds, sunflower seeds, and popcorn should be avoided, especially during an active flare-up. However, some people may tolerate small amounts if they chew thoroughly.
7. Sugary Foods
Sugary foods can contribute to inflammation and digestive issues, worsening symptoms of diverticulitis.
- Examples: Sweets, candies, and sugary drinks should be limited. Opt for natural sweeteners like honey or fruit if you need to add sweetness to your diet.
For a more detailed list of foods to avoid with diverticulitis, you can visit this comprehensive guide on foods to avoid with diverticulitis.
Foods to Include in Your Diet
Including the right foods in your diet supports digestive health and helps manage diverticulitis symptoms.
1. High-Fiber Foods
High-fiber foods promote healthy digestion and prevent constipation, reducing the risk of diverticulitis flare-ups.
- Examples: Whole grains like brown rice, quinoa, and whole wheat bread; fruits like apples, pears, and berries; and vegetables like broccoli, carrots, and spinach are excellent sources of dietary fiber. Aim for at least 25-30 grams of fiber daily.
2. Lean Proteins
Lean proteins provide essential nutrients without irritating the digestive tract.
- Examples: Chicken, turkey, fish, and plant-based proteins like tofu and legumes are good choices. These proteins are easier to digest and less likely to cause inflammation.
3. Low-Fat Dairy Alternatives
If you tolerate dairy, opt for low-fat or lactose-free alternatives to reduce fat intake and support digestive health.
- Examples: Low-fat milk, yogurt, and cheese are better options than full-fat dairy products. Lactose-free varieties are available for those with lactose intolerance.
4. Hydrating Foods
Hydrating foods help maintain fluid balance and support digestive function.
- Examples: Cucumbers, watermelon, and citrus fruits are hydrating and provide additional vitamins and minerals. Ensure adequate fluid intake by drinking plenty of water throughout the day.
5. Probiotic-Rich Foods
Probiotic-rich foods support gut health by promoting a healthy balance of gut bacteria.
- Examples: Yogurt with live cultures, kefir, sauerkraut, and kimchi are good sources of probiotics. These foods can help maintain gut health and reduce inflammation.
6. Healthy Fats
Healthy fats from sources like nuts, seeds, and olive oil support overall health and can be included in moderation.
- Examples: Avocados, nuts (if tolerated), and seeds (if tolerated) provide healthy fats that support hormone production and cell function. Use olive oil for cooking and salads.
Tips for Managing Diverticulitis Through Diet
In addition to choosing the right foods, adopting certain dietary practices helps manage diverticulitis and maintain digestive health.
1. Gradual Fiber Increase
Increase fiber intake gradually to prevent gas and bloating. Abrupt changes in fiber consumption can cause digestive discomfort.
- Step-by-Step Increase: Start with small amounts of high-fiber foods and gradually increase the quantity over several weeks. This approach allows your digestive system to adjust.
2. Stay Hydrated
Drinking plenty of water supports digestion and helps prevent constipation, which can exacerbate diverticulitis symptoms.
- Daily Water Intake: Aim for at least 8-10 glasses of water daily. Adjust your intake based on activity level, climate, and overall health.
3. Eat Smaller, Frequent Meals
Eating smaller, frequent meals helps manage digestive symptoms and reduces the risk of flare-ups.
- Meal Frequency: Instead of three large meals, try eating 4-6 smaller meals throughout the day. This approach keeps your digestive system active and prevents overloading it at any one time.
4. Avoid Triggers During Flare-Ups
Identify and avoid trigger foods that exacerbate symptoms during diverticulitis flare-ups.
- Flare-Up Diet: During flare-ups, stick to a low-fiber, bland diet to minimize irritation. Gradually reintroduce high-fiber foods as symptoms improve.
5. Chew Thoroughly
Chewing food thoroughly aids digestion and reduces the risk of irritating the digestive tract.
- Eating Mindfully: Take your time to chew food well before swallowing. This practice helps break down food and makes it easier for your digestive system to process.
6. Monitor Symptoms
Keep a food diary to track your diet and symptoms. This practice helps identify foods that trigger symptoms and allows for better management.
- Symptom Tracking: Record what you eat and note any symptoms that occur. Look for patterns that suggest certain foods or eating habits are causing issues.
When to Seek Medical Help
While dietary management often helps control diverticulitis, it’s crucial to know when to seek medical help for more serious symptoms.
Persistent Symptoms
Consult a healthcare provider if you experience persistent symptoms that do not improve with dietary changes. Persistent pain, fever, or significant changes in bowel habits may indicate complications.
Severe Symptoms
Seek immediate medical attention for severe symptoms, such as intense abdominal pain, high fever, or signs of infection. These symptoms could signal a serious flare-up or complication requiring medical intervention.
Regular Check-Ups
Schedule regular check-ups to monitor your condition and adjust your diet as needed. Discuss any concerns or changes in symptoms with your healthcare provider for ongoing management.
Conclusion
Understanding diverticulitis and managing it through diet is essential for alleviating symptoms and preventing flare-ups. By avoiding certain foods, incorporating beneficial ones, and adopting healthy eating practices, you can effectively manage diverticulitis and maintain digestive health. Whether dealing with occasional flare-ups or managing chronic symptoms, a well-planned diet supports your overall well-being and helps you lead a more comfortable life.
For more detailed information on foods to avoid with diverticulitis, visit this comprehensive guide on foods to avoid with diverticulitis.
